Pregnancy and Fat Loss-13 Expert Tips to Do It Safely
(This post probably contains affiliate links. I receive a small commission at no cost to you through links shared on this website to help keep the information I provide free to you)
Congratulations on your pregnancy! As a mom of four, I know first-hand how scary and uncertain this time can feel.
And if you are starting your pregnancy overweight, the thought of gaining more weight may feel extremely overwhelming and scary.
But should fat loss during pregnancy be your goal?

Weight management during pregnancy can be complicated and it depends on multiple factors such as BMI (body mass index) before conception, activity level, type of exercise if any during pregnancy, age, and whether there are existing medical conditions.
Today we will explore what the research shows us about fat loss during pregnancy and if it is safe for you and your pregnancy.
We will also discuss safe methods to avoid weight-related complications in pregnancy.
Disclaimer: This website and information provided is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Struggles of a Fit Mom uses only high-quality sources and the content is for informational and educational purposes only.
What Are the Risks of Being Overweight or Obese During Pregnancy?
Obesity is a complex, sensitive, and increasing worldwide health problem with increasing numbers of women of reproductive age being affected by it.
Unfortunately, being overweight or obese during pregnancy can affect the immediate and future health of a woman and her infant.
These risks include:
High Blood Pressure
When blood pressure increases, it places excess pressure against the walls of your arteries.
This can cause extra stress on your heart and kidneys, leading to serious pregnancy complications such as preeclampsia, preterm birth, low birth weight, and cesarean birth.
Preeclampsia
Preeclampsia is a condition associated with abnormally high blood pressure and could be an indication of organ system damage, particularly the liver and kidneys.
It is a major contributor to maternal and neonatal mortality and morbidity affecting 5% to 7% of pregnant women worldwide.
Preeclampsia is dangerous for you and your baby because this increased blood pressure can restrict blood flow to the placenta which means less oxygen and nutrients for your baby.
Many women still deliver healthy babies if preeclampsia is caught early enough and treated appropriately by your healthcare provider.
Gestational Diabetes
Diabetes is a condition where blood sugar rises to unhealthy or dangerous levels because the body cannot produce enough insulin or the cells are resistant to the insulin produced.
Gestational diabetes is a form of diabetes that only affects pregnant women and typically goes away after pregnancy.
When blood sugar levels stay high over time, it can lead to serious pregnancy complications such as preeclampsia, preterm birth, cesarean section, macrosomia (large baby) and even stillbirth.
Complications during labor and delivery
Overweight pregnant women may be at greater risk for complications during labor and delivery including cesarian sections, preterm delivery, infection from improper wound healing, longer labors.
If you do have a c-section, the risks of infection, improper wound healing and other complications are greater in overweight or obese women.
Inaccurate Fetal Testing
Carrying excess body fat can interfere with with accuracy of certain prenatal screening tests such as ultrasounds and difficulty checking the baby’s heart rate with a fetal doppler.
Fatigue
Pregnant women who are struggling with obesity may experience more fatigue during pregnancy because their bodies are working harder to keep up with extra weight.
Fatigue can lead to moms not take good care of themselves or their babies as much as they should.
It can also make it more difficult for moms to complete day-to-day responsibilities such as prepare food and meals, get proper rest and relaxation, and care for their babies before and after birth.
Miscarriage
Unfortunately, obesity is associated with an increased risk of early pregnancy loss and recurrent miscarriage.
This is because carrying excess body fat increases your risks of complications such as preeclampsia and difficulty managing diabetes.
How Do I know if I’m Overweight or Obese During Pregnancy?
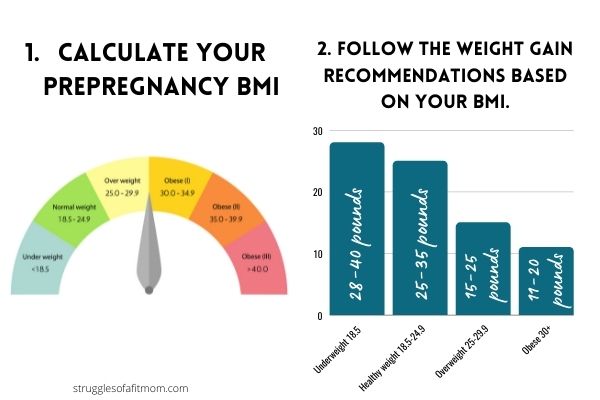
Calculating your Body Mass Index (BMI) will tell you your risk of obesity during pregnancy.
This is the measurement of your height relative to your weight.
Calculating your BMI is the most accurate predictor of obesity-related risk during pregnancy and can be a helpful tool for healthcare providers as well.
A higher BMI prior to or during pregnancy places you at greater risk for health complications including preeclampsia, gestational diabetes, preterm birth and blood clots.
BMI Scale:
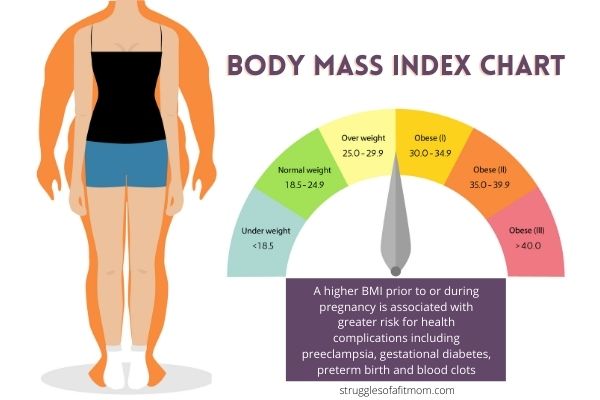
I know it can be difficult to receive your BMI results but try not to be upset or offended if your healthcare provider uses any of these terms to describe your weight.
These are the medical terms they need to uses they they can make sure you get the best advice and support for a healthy pregnancy.
You can determine your BMI by using an online calculator or ask your doctor to do it for you.
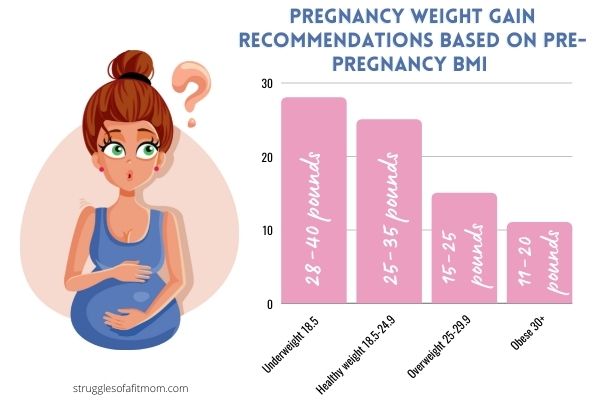
What is the Recommended Weight Gain Requirements if You Are Pregnant and Overweight?
We cannot look at weight gain during pregnancy as a one size fits all approach but rather as a spectrum with multiple considerations to be taken into account.
How much weight you should gain during pregnancy is primarily determined by your pre-pregnancy body mass index or BMI.
If you begin pregnancy overweight or obese, the recommended total weight gain will be less than those of a normal BMI.
This is because overweight women have a higher calorie reserve in the formed of stored fat.
Too much or too little weight gain can also cause health risks to you and your baby.
It is important to work closely with your health care provider to make sure you gain enough weight for your pregnancy.
Weight gain recommendations during pregnancy from the American College of Obstetricians and Gynecologists:
- Underweight pre-pregnancy (BMI less than 18.5)- 28-40 pounds
- Average prepregnancy weight (BMI 18.5-24.9): 25-35 pounds
- Overweight pre-pregnancy (BMI 25-29): 15-25 pounds
- Obese prior to pregnancy (BMI 30+)- 11-20 pounds (1)
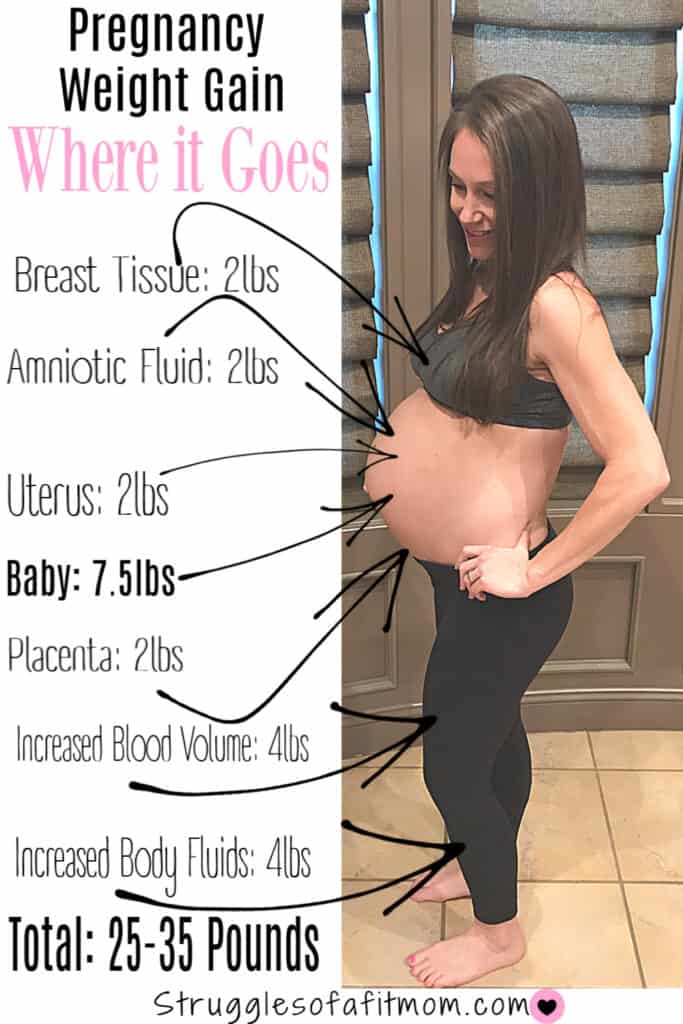
Distribution of Weight Gain During Pregnancy
So you’re probably wondering where all the weight gain goes if your baby is only about 7.5 pounds, right?
- Breast tissue: 2lbs
- Uterus: 2 lbs
- Placenta and amniotic fluid: 4 lbs
- Baby: 7.5 lbs
- Increased blood volume: 4lbs
- Increased body fluids: 4 lbs
- Extra body fat stores: 6-8 pounds
These are only rough estimates and may vary with each person or pregnancy.
Is Fat Loss During Pregnancy Safe?
If you are overweight or obese, should fat loss during pregnancy be your focus?
Experts warn against intentional weight loss during pregnancy, even in obese patients.
This is because drastically reducing calories or dieting is not healthy for you or your pregnancy because it can deprive your baby of essential nutrients.
However, if you have changed your eating habits since becoming pregnant, are consuming enough calories for you and your baby and are losing some weight, this shouldn’t be a reason for concern.
If you are someone who is overweight during pregnancy, fat loss should not be your goal but rather focusing on preventing excess weight gain.
What About Unintentional Weight Loss During Pregnancy?
Weight loss during pregnancy is not always a reason for concern.
Many moms experience morning sickness, nausea and food aversions in the first trimester which can cause some early weight loss.
This is not usually a reason for concern but it should still be monitored by your doctor.
Luckily, morning sickness usually resolves in most women by second trimester.
If you are concerned about losing weight during pregnancy, make sure to speak to your health care provider.

Is Dieting During Pregnancy Safe?
The definition of dieting is to “restrict oneself to small amounts or special kinds of food in order to lose weight.”
This means that dieting during pregnancy, especially crash diets, is not recommend.
For example, if you want to cut out carbohydrates thinking it will help you lose weight, you may be restricting essential nutrients from fruit and whole grains.
Dieting is strongly discouraged during pregnancy and instead, your focus should be on developing healthy eating habits and preventing excess weight gain.
How to Lose Weight or Prevent Excess Weight Gain During Pregnancy
If you and your healthcare provider determine that weight loss during your pregnancy is healthy and beneficial for both you and your baby, here are some tips to help you reach your goals while ensuring your baby’s growth is steady.
1. Determine Your Weight Gain Requirements
Use the BMI chart to determine your overall weight gain needs during your entire pregnancy.
Then discuss these goals with your healthcare provider to make sure you are getting the support and resources you need to stay within your weight gain requirements.
2. Understand Your Calorie Requirements
Next, understand your calorie intake requirements during pregnancy.
The average number of calories an expecting mom needs during pregnancy is at least 1700.
However, this number will vary from person to person based on age, activity level, weight and genetics.
Most women do not need any extra calories during pregnancy until the second and third trimester.
If you are overweight or obese and not gaining weight but your baby shows adequate weight gain, then you probably don’t need to consume extra calories because the baby is getting what they need.
3. Track What You Eat
Use an app on your phone, or simply write keep a written journal of what you are eating.
But make sure you are being honest and documenting accurately!
This way you can track your calories and see if it is within your needs.
One study for Cornell University stated that overweight or obese individuals underestimate their caloric intake by as much as 40%!
Mose struggle with weight loss because they significantly underestimate how many calories they consume and over estimate the number of calories their body burns.
Tracking what you eat will help you to better understand your body’s caloric needs.
4. Track Your Weight
I still struggle with stepping on the scale even after 4 babies!
But this is essential to ensuring you are gaining a healthy amount of weight for both you and your baby.
Avoid weighing yourself more than once a week because your weight can fluctuate due to water retention, constipation and many other factors.
And try not to stress too much. Stress is not good for you or your baby.
Use this free tracker to monitor weekly weight loss or gain.
5. Keep A Pregnancy Journal
Journaling and documenting your pregnancy can be very therapeutic.
You can write down how you are feeling, any changes in your body and even words of encouragement to yourself!
This can be a great reminder of what you have accomplished throughout the course of your pregnancy.
It will also help you monitor your weight, diet and baby growth as well to give you some peace of mind in your journey.
And take bump pictures every week so you have something to look back on in the future.
6. Get Support From Others
If you find yourself struggling with weight management, don’t be afraid to ask for help!
Whether it’s asking for a referral to a nutritionist, a community group or even family and friends.
Having support is essential in helping you stay on track with your goals!
7. Avoid Following a Weight Loss Diet
Rigorous weight loss diets such as intermittent fasting or meal plans that eliminate entire food groups should be avoided completely during pregnancy.
The last thing you want to do is deprive your developing baby of essential nutrients!
8. Chose Food Quality Over Quantity
There is a HUGE myth that pregnant moms need to “eat for two”.
This mindset only sets moms up for failure in thinking that in order to have a healthy pregnancy, the need to drastically increase their food consumption.
Instead, focus on improving food quality over food quantity.
Eating for two means ensuring your are getting a variety of healthy nutrients including lean protein, whole grains and reducing processed foods that provide little to no nutritional value.
You may even lose a few pounds simply by eating a more healthy and balanced diet but drastically restricting calories or food groups is not recommended.

9. Get Enough Physical Activity
While I would never recommend exercising with the intent of losing weight during pregnancy, movement truly is medicine!
Current research shows that for most moms, the benefits of staying active during pregnancy far outweigh the risks, even if you have never exercised before.
Studies show that prenatal exercise can help decrease lower back pain, pelvic pain, constipation, bloating and swelling.
And the best part? It can help your body prepare for an easier and faster labor and delivery!
The American College of Obstetricians and Gynecologists recommends getting at least 150 minutes of moderate exercise a week. This is about 30 minutes a day.
You can safely exercise during pregnancy, even if you have never been active before.
Of course you need to discuss this with your doctor.
Related: These 25 Benefits of Exercise During Pregnancy Will Motivate You to Move

10. Hydrate
I cannot stress the importance of drinking enough water.
Not only will staying hydrated help keep cravings at bay, dehydration may lead to dizziness, headaches or light headedness which can be dangerous for you and your baby.
And later in pregnancy, dehydration can cause contractions.
Aim to consume at least 8-12 cups per day (ACOG).
11. Take a Prenatal Vitamin
Moms need more nutrients during pregnancy than ever before.
This is why I ALWAYS recommend taking prenatal vitamins to fill in the gaps and be sure you are getting all of the vital nutrients your body needs for both you and baby.
12. Accept The Changes
Remember, pregnancy is temporary and your body will go back to its pre-pregnancy state soon enough.
The more accepting you are of the changes your body goes through, the better chance you have of having a healthy delivery and smooth recovery.
Related: 15 Tips to Overcome Negative Body Image During Pregnancy
13. Focus on Creating a Healthy Lifestyle
The best way to make sure you are giving your baby all the nutrients they need without going too far in either direction is to focus on healthy eating habits, self-care and a positive attitude.
This includes getting enough sleep, reducing stress, exercising and replacing processed foods with foods that are more nutritionally dense like whole grains, lean protein, fruits and vegetables.
Don’t become overly preoccupied with numbers and rules. This will only be counter-productive.
Remember, pregnancy should not be used as an opportunity to lose weight but rather an opportunity to create healthier lifestyle habits for both you and your baby.
How Can I Avoid Getting Fat During Pregnancy?
As per the guidelines set by the American College of Obstetrics and Gynecology , every pregnant woman needs to gain weight during pregnancy, irrespective of their BMI.
Before you panic about the number on the scale, focus on fueling your body with nutrient dense foods.
Your focus should not be on fat loss during pregnancy but rather preventing excess weight weight gain by minimizing processed junk food, getting good sleep, staying active and staying hydrated.
Making small lifestyle changes may even help you unintentionally loose a few pounds.
Can I Still Have a Healthy Pregnancy if I am Overweight or Obese?
Absolutely!
Despite the risks listed above, many moms have healthy pregnancies and babies.
However, it does require careful monitoring by your health care team, special considerations during labor and delivery and following a healthy diet and exercise program.
Related: Can You Exercise During Pregnancy if You Are Overweight or Obese?
Final Thoughts on Fat Loss During Pregnancy
Fat loss while pregnant can be safe if it is recommended by your healthcare provider and part of an overall healthy lifestyle that includes proper nutrition, exercise and other efforts to prevent excessive weight gain.
You may be wrestling with poor body image or the fear of early pregnancy loss due to being overweight or obese but the number one most important thing to focus on your health the baby’s health.
Despite the risks of being overweight or obese during pregnancy, intentional weight loss during pregnancy is very individualized and should only be done under the recommendation and supervision of your healthcare team.
I am only one email away if you need support, motivation or tips to help you through your pregnant journey!
Sources
FACT CHECK
Struggles of a Fit Mom uses only high-quality sources, including peer-reviewed studies, to support the facts within it’s articles. Read my editorial process to learn more about how I fact-check and keep my content accurate, reliable, and trustworthy.
Peer reviewed studies
https://americanpregnancy.org/healthy-pregnancy/pregnancy-complications/preeclampsia/
https://www.marchofdimes.org/pregnancy/being-overweight-during-pregnancy.aspx
https://www.nhs.uk/conditions/obesity/
Kominiarek MA, Rajan P. Nutrition Recommendations in Pregnancy and Lactation. Med Clin North Am. 2016;100(6):1199-1215. doi:10.1016/j.mcna.2016.06.004

Brooke is a certified Prenatal and Postnatal Exercise Specialist with a Bachelors of Science degree in Kinesiology-Exercise Science. She is also a mom of 3 girls with more than 15 years of experience in health and fitness. Brooke’s goal at Struggles of a Fit Mom is to help motivate, educate and inspire other busy mamas who struggle with finding time, energy and motivation to take care of themselves in the chaos of motherhood.